Breast engorgement
9-minute read
Key facts
- Breast engorgement is when your breast tissue overfills with milk, blood and other fluids.
- Your breasts may feel very full, hard, swollen and painful.
- Your nipples can become flat, and it might be difficult for your baby to attach.
- Feeding your baby on demand will help your body to adjust the amount of milk you make.
- If emptying the breast does not help with pain from breast engorgement, see your doctor, midwife, lactation consultant or child and family health nurse.
What is breast engorgement?
Breast engorgement is when your breast tissue overfills with milk, blood and other fluids.
When your baby is born, your breasts are given a signal to start full milk production. Your milk usually starts around 2 to 3 days after your baby is born. Breast engorgement that occurs in the first few days after your baby is born is known as ‘physiological engorgement’. It is quite common and usually resolves on its own with effective breastfeeding.
Breast engorgement can also happen at any time when you are breastfeeding or expressing breast milk, especially if your baby’s sleeping or feeding patterns change and they feed less than usual. It can also occur if you have an oversupply of breast milk. Breast engorgement that happens after you have already established breastfeeding is known as ‘secondary’ or ‘pathological engorgement’.
What are the symptoms of breast engorgement?
Engorgement can make your breasts feel very full, hard, swollen and painful. Engorgement happens in both breasts at once.
Your nipples might become stretched, or flat and tight. This can make it difficult for your baby to attach to the breast.


What causes breast engorgement?
Breast engorgement can happen if your body makes more milk than your baby is drinking.
This might occur if:
- your baby is not attaching and feeding well
- your baby misses a feed
- you are feeding your baby on a schedule and not ‘on-demand’
- you are combining breastfeeding with bottle-feeding (‘mixed feeding’)
- you are feeding your baby expressed breast milk, and are expressing more than your baby is drinking
How can I relieve breast engorgement?
If your breasts become engorged and painful, there are things you can do to relieve the discomfort and reduce the chance of complications.
The best thing to do is to empty the breast, ideally by letting your baby feed at the breast. If you are having trouble attaching your baby due to the engorgement, or it is too uncomfortable, you can try expressing a small amount of breast milk by hand to soften the breast and, waking your baby and offering a breastfeed day or night if your breasts become uncomfortable between feeds.
You don’t need to breastfeed or pump until your breast is empty. If you continue to breastfeed your baby on-demand, the engorgement will usually resolve. Your body will learn to produce the right amount of milk for your baby, reducing the chance of future episodes of engorgement.
If you are feeding your baby expressed breast milk, only express as much as you expect your baby to drink. This will help you avoid oversupply, which can lead to engorgement.
These tips might also help you feel more comfortable:
Before a feed:
- Wear a well-fitting, supportive bra.
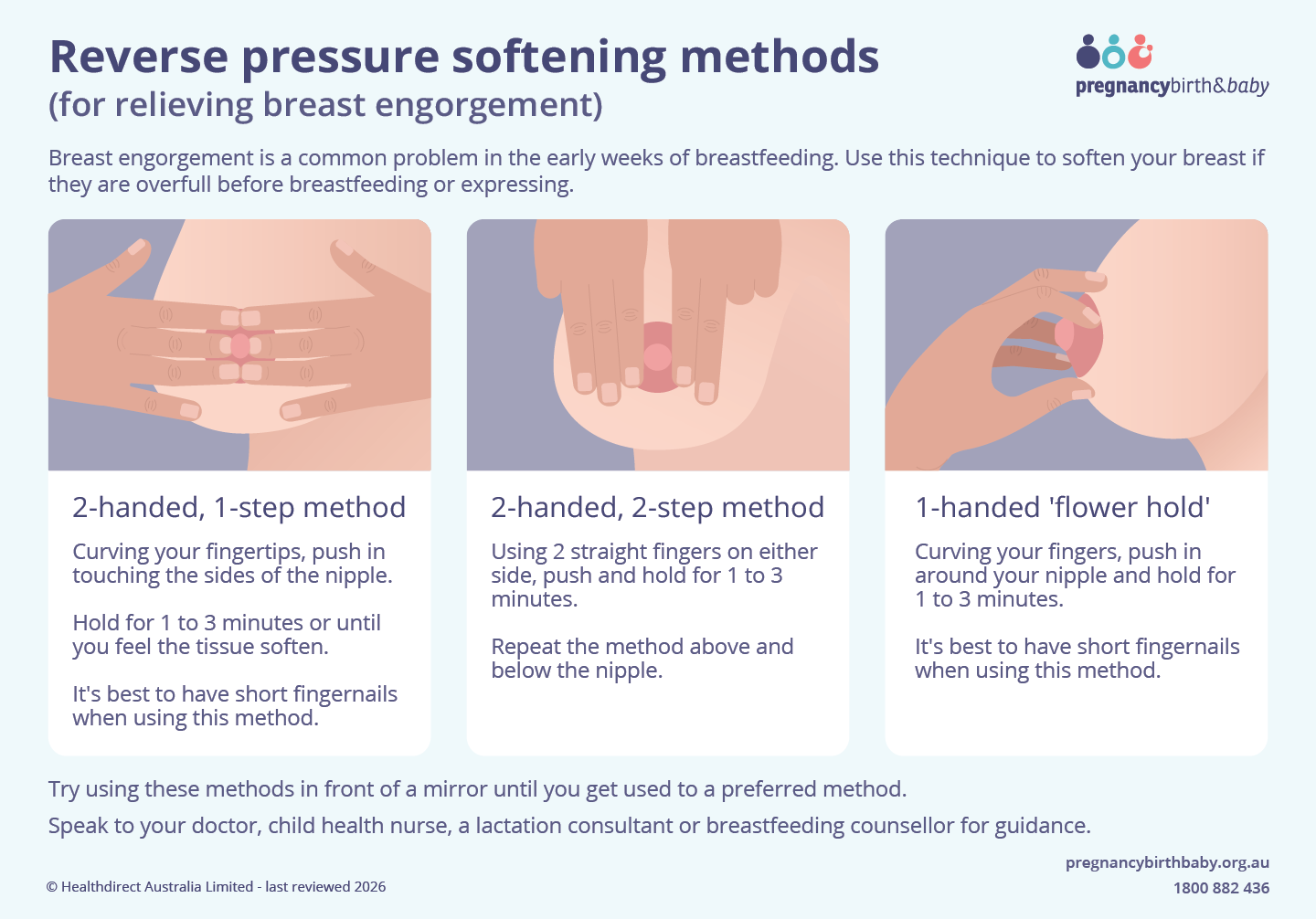
- Hand express a small amount of breast milk or try ‘reverse pressure softening’ (applying pressure around the nipples to push fluid back into the breasts).
- Take your bra off to help your baby attach more comfortably.
- Gently massage your breasts or use a warm compress to encourage milk flow.
After a feed:
- Use a cool pack from the fridge or a chilled, washed cabbage leaf over the breast to reduce inflammation.
- If your breasts still feel uncomfortably full, try hand expressing a little milk.
- Take an anti-inflammatory medicine, such as ibuprofen, if your doctor or pharmacist say it is suitable for you.
- Try to rest and reduce your stress levels as much as possible to reduce the risk of breast infection (bacterial mastitis).
If you are still uncomfortable, or you are concerned, see your doctor, midwife or lactation consultant for advice and support.
When should I see my doctor?
You should see your doctor if your breast engorgement doesn’t resolve with the self-care tips above. You should also see your doctor if:
- you are concerned that your baby is not attaching well to your breast
- you have a fever
- you are feeling generally unwell
- your symptoms affect only one breast
- you have a red, tender area or lump on your breast
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
What are the complications of breast engorgement?
If breast engorgement continues, it could lead to mastitis.
If your breast engorgement doesn’t resolve with the self-care tips above, you should see your doctor, midwife or lactation consultant for advice.
How can breast engorgement be prevented?
To reduce the chance of breast engorgement after breastfeeding has been established, you can try the following.
- Feed your baby often and on demand (not by the clock) from birth. Most babies need 8 to 12 feeds per day once your milk comes in on day 3 to 4. It helps to sleep in the same room as your baby to help you and your baby adjust to breastfeeding.
- Don’t limit your baby’s time at the breast. Let them feed for as long as they want.
- Wake your baby for a feed if your breasts become full and uncomfortable (especially at night).
- Ensure your baby is positioned correctly and attached well. Hand express a little, if needed, to help your baby attach well to your breast.
- Avoid giving your baby any fluids other than breast milk.
- Use a nipple shield only if recommended by your doctor, midwife or lactation consultant, as these can affect your baby’s attachment to your breast.
Resources and support
For advice and support with breast engorgement:
- Read more at Australian Breastfeeding Association or call their helpline on 1800 686 268.
- Ask your midwife, child health nurse, or your doctor.
- Visit the Lactation Consultants Australia and New Zealand’s website to find a lactation consultant.
Other languages
The Australian Breastfeeding Association has breastfeeding resources translated into a variety of community languages.
HealthTranslations Victoria has a booklet called ‘Breastfeeding your baby’ available in a variety of community languages.
Aboriginal and/or Torres Strait Islander peoples
The Australian Breastfeeding Association has breastfeeding resources for Aboriginal and/or Torres Strait Islander people.
Sexually and gender-diverse families
The Australian Breastfeeding Association has resources on breastfeeding, chestfeeding and human milk feeding. It has information and support for the LGBTQIA+ community, and aims to be inclusive of all LGBTQIA+ families.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: December 2024





