Postpartum endometritis
8-minute read
Key facts
- Postpartum endometritis is an infection in the lining of your uterus after you give birth.
- Symptoms include fever, tummy pain, feeling tender in the pelvis and smelly vaginal discharge.
- Postpartum endometritis is treated with antibiotics.
- Your chance of getting postpartum endometritis is higher after a caesarean section.
- Use of antibiotics and antiseptics before a caesarean can lower your chance of getting postpartum endometritis.
What is postpartum endometritis?
Postpartum endometritis is an infection in the lining of your uterus that happens after giving birth. Postpartum means ‘after birth’.
Your uterus (womb) is in the middle of your pelvis. The inner layer lining your uterus is called the endometrium.
Endometritis is when this lining becomes inflamed. This is usually caused by germs entering your uterus during birth. This can cause a bacterial infection.
Postpartum endometritis usually happens in the first week after giving birth. However, sometimes it can happen up to 6 weeks after giving birth.
Endometritis can also be unrelated to birth (chronic endometritis). This may be due to pelvic inflammatory disease — an infection and inflammation of the uterus and ovaries. It causes scarring in these areas. Sexually transmitted infections are the most common causes of pelvic inflammatory disease.
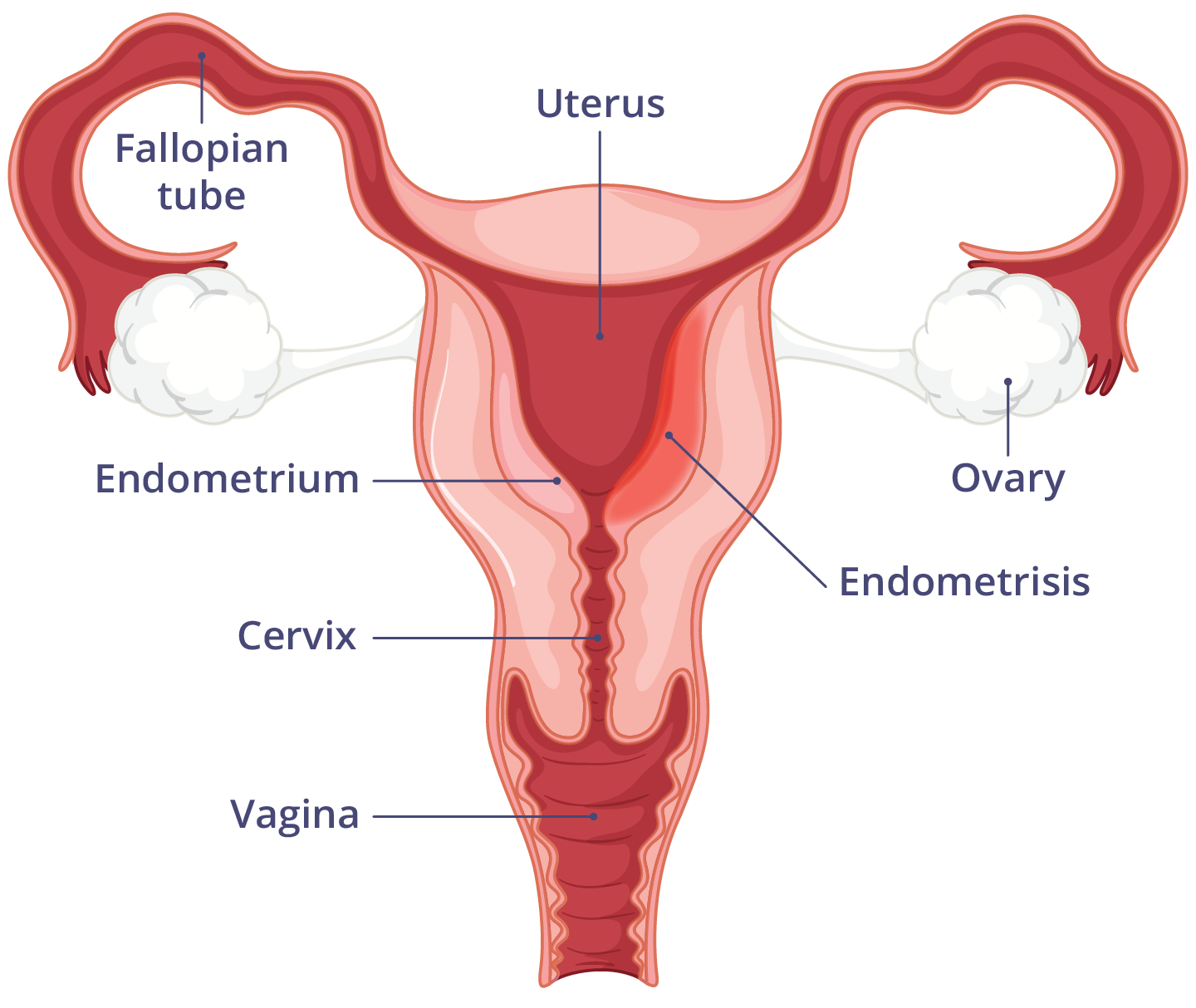
How is postpartum endometritis different from endometriosis?
Endometriosis is when tissue from the lining of your uterus grows in other parts of your body. Symptoms of endometriosis are:
Postpartum endometritis is an infection in the lining of your uterus.
What are the symptoms of postpartum endometritis?
The symptoms of postpartum endometritis are:
- fever — a temperature over 38°C
- tummy pain — due to swelling of the endometrium
- feeling tender in your pelvis
- smelly vaginal discharge
- an increase in bleeding from your vagina
If you notice any of these symptoms, call your doctor or midwife as soon as possible.
It can be hard to know what is normal after giving birth. Having some pain, vaginal bleeding and discharge is normal.
If postpartum endometritis happens later, it might be milder and appear as bleeding after giving birth.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes postpartum endometritis?
Postpartum endometritis happens when bacteria enter your uterus during childbirth.
Your uterus is free of bacteria until your waters break. This lets bacteria enter your uterus. These bacteria can cause an infection in the lining of your uterus.
Any woman can get postpartum endometritis.
Research shows that it affects up to:
- 3 in 100 women after a vaginal birth
- 1 in 3 women after a caesarean birth
Things that increase your chance of getting postpartum endometritis are:
- a long time between your ‘waters breaking’ and delivery of your baby
- multiple checks of your vagina during childbirth
- infection during pregnancy
- postpartum haemorrhage
- anaemia
Endometritis is more likely if your uterus wall is damaged through surgery.
When should I see my doctor?
See your doctor if you think you have an infection after giving birth.
Your doctor may refer you to an obstetrician.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is postpartum endometritis diagnosed?
Your doctor will ask you about your symptoms and might examine you. To confirm the cause of your infection, they may do a:
- vaginal swab
- blood test
- urine test
How is postpartum endometritis treated?
Most women with postpartum endometritis get better quickly with antibiotics. You should start feeling much better within a few days of starting the antibiotics.
Your treatment will match the severity of your condition. Your doctor will decide which antibiotic is best for you. This is based on:
- your symptoms
- other medicines you take
- any allergies
- your test results
Mild postpartum endometritis
If you have a mild infection, you may be treated at home.
Postpartum endometritis is considered mild if:
- your infection is in a specific area of your body
- you do not have fever
- you do not have lots of symptoms
Oral antibiotics are usually given for mild infections.
Severe postpartum endometritis
If your postpartum endometritis is severe, your doctor will care for you in a hospital.
You need to be treated quickly with antibiotics.
They will give you intravenous antibiotics (into your vein).
You may also be given oxygen.
Postpartum endometritis is considered severe if you have:
- lots of symptoms
- sepsis or septic shock
What are the complications of postpartum endometritis?
Postpartum endometritis can lead to sepsis, which is a medical emergency and can be fatal if not treated quickly. If you suspect you or someone else has sepsis, call triple zero (000) and ask for an ambulance.
Complications of postpartum endometritis are usually rare. However, they can happen if the infection is not treated quickly.
It can cause serious complications such as:
- sepsis — inflammation of your whole body
- peritonitis — an infection of the membrane inside your abdomen
- pelvic abscess — in the area below your belly button
- blood clots — in your veins, pelvis or lungs
Can postpartum endometritis be prevented?
If you have a caesarean section, your doctor may offer you intravenous (IV) antibiotics. This lowers your chance of getting an infection.
Will postpartum endometritis affect my future pregnancies?
Quick treatment of postpartum endometritis usually prevents any long-term problems.
If an infection is left untreated for too long, it may cause complications. This can lead to infertility.
Resources and support
If you think you may have postpartum endometritis, call your doctor or midwife straight away.
RANZCOG has a resource on what to expect in the first few weeks after birth.
ForWhen connects new and expecting parents with perinatal and infant mental health services and support in their local area. Contact the service on 1300 24 23 22.
Birth Trauma Australia offers advice, resources and a peer-to-peer support program.
The Centre of Perinatal Excellence (COPE) offers information and has a list of support services.
Perinatal Anxiety & Depression Australia (PANDA) supports parents and families during pregnancy and throughout the first year of parenthood. Call the helpline on 1300 726 306 to speak with a counsellor.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: February 2025




