Anatomy of pregnancy and birth - uterus
7-minute read
Key facts
- Your uterus (also known as your womb) sits in the middle of your pelvis.
- During your pregnancy your uterus grows and undergoes several changes.
- The size of your uterus is monitored during pregnancy.
- During labour, your uterus contracts regularly to open your cervix and help your baby move down into the birth canal.
- After you have had a vaginal or caesarean birth, your uterus will have contractions to help it shrink.
What is the uterus?
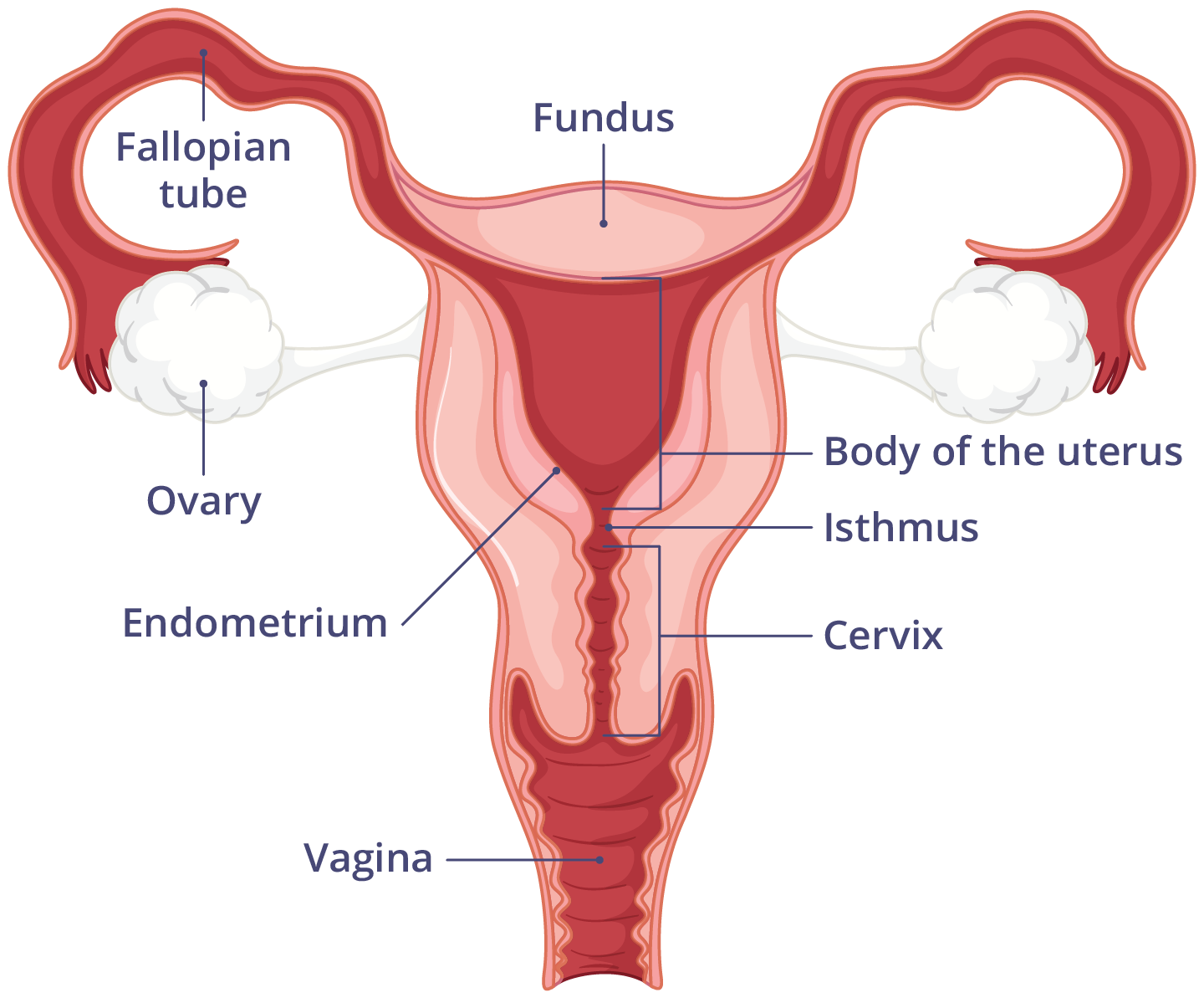
Your uterus (also known as your womb) sits in the middle of your pelvis. It is pear-shaped and has 4 main parts:
- fundus — the top of your uterus
- corpus — the main body of your uterus
- isthmus — the section between the main body of your uterus and cervix
- cervix — the lower part of your uterus, which connects to your vagina
Ligaments (bands of tough, flexible tissue) hold your uterus in place. It sits behind your bladder and in front of your rectum.
The wall of your uterus is made up of 3 layers:
- an inner layer called the endometrium, which responds to hormones. When you have your period, you shed this layer.
- a middle layer that is made of muscle
- a thin outside layer
How big is my uterus?
The size and shape of your uterus change throughout your life, depending on your age and stage of life. As you reach menopause, your uterus will become smaller.
How does my uterus change during pregnancy?
During pregnancy, as your baby grows, your uterus will greatly increase in size.
Fundal height
Fundal height is the distance from your pubic bone (at the front of your pelvis) to the top of your uterus. Your doctor, obstetrician or midwife may measure your fundal height at each antenatal visit from 24 weeks onwards.
Several factors can affect the size of your uterus. For instance, the fundal height may be different in people:
- who are carrying more than one baby
- living with overweight or obesity
- living with certain health conditions
A smaller than expected fundal height could be a sign that your baby is growing slowly or that there is too little amniotic fluid. If so, your doctor will carefully monitor you and your baby.
In contrast, a larger than expected fundal height could mean there is a chance your baby is larger than average. Your doctor will carefully monitor you and your baby.
If there are concerns about your baby’s growth, your doctor or midwife may recommend having ultrasound scans to monitor your baby.
How does the uterus prepare for labour and birth?
Your uterus prepares for labour and birth by doing Braxton Hicks contractions, also known as ‘false labour’ or ‘practice contractions’. Braxton Hicks contractions do not dilate (open) your cervix. You may feel a weak or uncomfortable tightening or ache around your baby bump for 20 – 90 seconds.
Braxton Hicks occur throughout your pregnancy. They may become more intense or frequent towards the end of your pregnancy. You may not feel them until the second trimester.
You can tell Braxton Hicks contractions from ‘real labour’ as they disappear when you change position or activity.
What happens to my uterus during labour?
During active labour, the muscles of your uterus contract to open your cervix and help your baby move down into the birth canal.
Labour contractions start like a wave moving from the top of your uterus right down to your cervix. They get stronger and stronger. Your uterus will feel tight during a contraction. Between contractions, the pain will ease off and allow you to rest before the next contraction builds.
Unlike Braxton Hicks, labour contractions become stronger, more regular and more frequent in the lead up to giving birth.
How does my uterus change after birth?
If you have a vaginal birth, your uterus will contract again to deliver your placenta. These contractions are milder than the contractions you felt during labour.
If you have a caesarean birth, your baby and placenta are delivered through a cut in your tummy and the wall of your uterus. Your uterus is then stitched up and will form a scar.
After your birth is completed, whether you had a vaginal or caesarean birth, your uterus will continue to have contractions. You may feel contractions when you breastfeeding.
The contracting and tightening of the uterus will feel a little like period pain and is also known as 'afterbirth pains'. These contractions help the uterus to reduce in size.
Read more here about the first few days after giving birth.
Resources and support
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists has an informative handout to help prepare you for labour and birth.
- Visit the Jean Hailes website to read more about your uterus.
- COPE, the Centre of Perinatal Excellence provides emotional support and tips to look after yourself for people expecting a baby and new parents.
- Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available from 7 am to midnight (AET), 7 days a week (including public holidays).
Aboriginal and/or Torres Strait Islander peoples
- You can find out more about Aboriginal and/or Torres Strait Islander pregnancy health on Stronger Bubba Born or watch the How to Have a Safer Pregnancy video.
Sexually and gender-diverse families
- The Gidget Foundation Australia provide perinatal support to sexually and gender-diverse families.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2024



