Fibroids and fertility
7-minute read
Key facts
- Fibroids are common, non-cancerous growths of muscle which form in the wall of the uterus (womb).
- Most people with fibroids have normal fertility and pregnancy outcomes.
- Fibroids don't always cause symptoms or need treatment.
- Fibroids can vary in size, number and location.
- There is a range of treatment options for fibroids, depending on the symptoms they cause.
What are fibroids?
Fibroids are common, non-cancerous growths found in the muscle wall of the uterus (womb). They are also called leiomyomas or myomas.
What you may experience depends on the type and size of your fibroids.
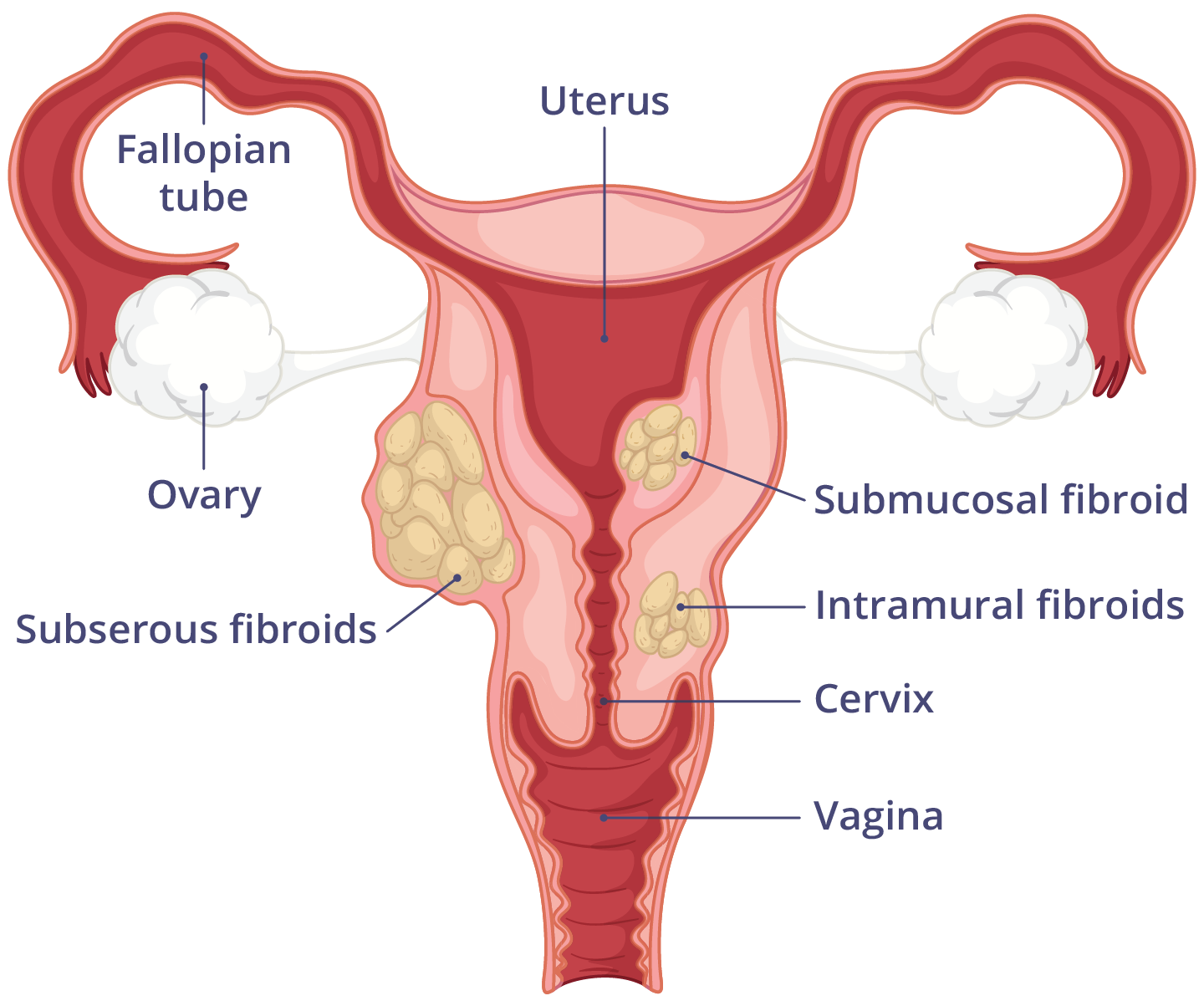
What are the different types of fibroids?
There are 3 types of fibroids, based on which layer of the uterus they grow in:
- Intramural fibroids grow in the uterine muscle.
- Subserous or subserosal fibroids grow in the outer muscle layer.
- Submucosal fibroids grow in the cavity of the uterus.
What are the symptoms of fibroids?
Many people don't know they have fibroids, unless they have symptoms, or the fibroids are seen during a scan. It's estimated that 1in 3 females experience symptoms.
Symptoms of fibroids can include:
- heavy or long periods, which can cause iron deficiency and anaemia
- painful periods
- painful sex
- bleeding between periods
- a feeling of heaviness in your back, bowel and bladder
- passing urine (wee) a lot
What causes fibroids?
The exact cause of fibroids is unknown. The growth of fibroids depends on the hormones oestrogen and progesterone. Fibroids grow in females of reproductive age until menopause.
Factors that increase your chance of developing fibroids include:
- getting your first period at an early age
- living with obesity
- a family history of fibroids
- never having given birth
- older age
- high blood pressure
- low vitamin D
Factors that lower your chance of fibroids include:
- having more than 2 births
- using Depo-Provera (medroxyprogesterone acetate) as a contraceptive
- taking the oral contraceptive pill
When should I see a doctor?
If you have been trying to conceive for 12 months (or 6 months if you are over 35 years old) and think you may have fibroids, it's a good idea to see a fertility specialist.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How are fibroids diagnosed?
If you have symptoms, your GP may send you for some tests, such as:
- vaginal ultrasound
- abdominal ultrasound
- magnetic resonance imaging (MRI)
Your GP may also send you for a laparoscopy or hysteroscopy, which use small cameras to look inside your pelvic organs and uterus.
How are fibroids treated?
Most fibroids don't need treatment unless they are causing problems. You might choose to seek treatment if you are experiencing:
- fertility problems
- period pain
- heavy bleeding
- pressure symptoms
Treatment options depend on the type of fibroids and symptoms experienced. It is also important to consider if there are plans for future pregnancies.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
Medical options
Pain relieving medicines such as anti-inflammatories may help with pain and heavy bleeding.
A Mirena IUD® releases the hormone progesterone to help reduce heavy bleeding.
The combined oral contraceptive pill can also help to reduce bleeding. These both need to be stopped if pregnancy is planned.
Medicines called GnRH agonists are artificial hormones that prevent natural ovulation. This can help reduce the size of fibroids before a planned operation. Once these hormones are stopped, fibroids can grow back.
Sometimes a combination of hormones is prescribed, which helps to shrink the fibroids, especially if fertility is affected.
If you have anaemia, you may be recommended to take iron replacement.
Surgical options
There are different surgical options to treat fibroids:
- Uterine artery embolisation injects small particles to block blood from reaching the fibroids. Not having a blood supply makes the fibroids shrink.
- Myomectomy is when a fibroid is removed during surgery under general anaesthetic. The surgeon may operate through the uterus or abdomen, depending on where the fibroid is.
- MRI-directed ultrasound is when ultrasound waves are used to overheat fibroid cells and shrink them.
- Hysterectomy is when the uterus is completely removed.
Can fibroids affect my fertility and pregnancy?
Many people with fibroids have normal fertility and pregnancy outcomes. Only certain types of fibroids will affect getting pregnant or birth. For example, large fibroids may change the baby's position and ability to move freely.
However, people with fibroids may also have higher rates of infertility and miscarriage. It is important to look at the size, location and number of fibroids. You are more likely to need a caesarean birth if you have fibroids.
Can fibroids be prevented?
There is no known way to prevent uterine fibroids. Doctors recommend you make healthy lifestyle choices, such as maintaining a healthy weight. Eating fruits and vegetables may also decrease your chance of fibroids.
Using hormonal contraceptives may lower your chance of fibroids.
Resources and support
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week (including public holidays).
Languages other than English
Jean Hailes has factsheets on topics such as heavy periods available in many community languages.
Your Fertility has factsheets on fertility available in several community languages.
Information for Aboriginal and/or Torres Strait Islander peoples
Jean Hailes has a booklet and video on periods, available for Aboriginal and/or Torres Strait Islander people.
Find an Aboriginal Community Controlled Health Organisation (ACCHO) or Affiliate near you.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2025




