Vaccinations and pregnancy
14-minute read
Key facts
- Vaccination is the process of getting a vaccine.
- Vaccination triggers immunisation in the body, which is your immune system’s response to the vaccine that helps protect you from the disease.
- Vaccination can protect both you and your baby from serious disease.
- Some vaccines are recommended before and during pregnancy, while others should be avoided.
- The Australian Immunisation Register records your and your baby’s vaccinations to help you remember what you’ve already had and what you need.
What is a vaccine?
Vaccines are medicines that contain a tiny amount of a virus or bacteria. After you get a vaccine, your body makes antibodies designed to attack that specific virus or bacteria. If you are exposed to the disease in the future, your body recognises it and can produce antibodies more quickly. This helps your body fight the disease more effectively, sometimes even before you develop symptoms of the disease.
The Therapeutic Goods Administration (TGA) approves vaccines for use in Australia. The TGA uses a strict process. This includes checking every ingredient in the vaccine for safety, quality and effectiveness.
Most vaccines are given by injection but some are given orally (by mouth).
Quick guide to vaccine terms
| Vaccine | A product made from dead or weakened germs (bacteria or viruses) that helps your body learn how to fight the infection. |
| Vaccination | The process of getting a vaccine. Vaccination triggers immunisation in the body. |
| Immunity | The body’s ability to fight infection. This may happen after infection or after vaccination. |
| Immunisation | The process of your body’s immune system learning how to protect you from an infectious disease. |
| ‘Booster’ dose | Extra vaccine doses given to strengthen immunity. |
| Herd immunity | When a large part of the population are vaccinated so people in the community are protected from a disease. |
How does immunisation work?
Immunisation is the process of your body’s immune system learning how to protect you from an infectious disease. Vaccination refers to when you receive the injection or oral dose of medicine.
Vaccination triggers immunisation in the body.
Is everyone protected from disease by immunisation?
When there are high vaccination rates, vaccine-preventable diseases become less common in the community. This means even someone who is not vaccinated is less likely to catch the disease. This is called herd immunity.
Herd immunity is important for people who can’t be or aren’t yet vaccinated, especially:
- babies and children who are too young for some vaccines
- babies and children who are still being vaccinated
- people who are allergic to some components of a vaccine
- those with a weakened immune system
Becoming immunised reduces the chance that these people will catch the disease.
If I’m planning a pregnancy, which vaccinations are recommended?
If you are planning to become pregnant, speak to your doctor about which vaccinations they recommend for you. They can check if you are up to date with certain vaccinations, such as:
- measles
- mumps
- rubella
- chickenpox (varicella)
- hepatitis B
- COVID-19
Having these vaccinations can help protect both you and your future baby from these diseases.
To see what vaccinations you’ve had, you can check your immunisation history statement on your myGov account or My Health Record, or ask your doctor.
Your doctor may refer you for a blood test to check your immunity levels against some of these diseases.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
What vaccinations are recommended during pregnancy?
Vaccinations strongly recommended during pregnancy include those against:
- flu (influenza), at any time during pregnancy
- whooping cough (pertussis), between 20 and 32 weeks of pregnancy. You can still have the vaccine after 32 weeks, but it’s best to get it earlier to protect your baby.
- respiratory syncytial virus (RSV), between 28 and 38 weeks of pregnancy. This can help protect your baby from RSV until they are 6 months old.
These vaccinations are free under the National Immunisation Program. To be eligible for NIP vaccines, you must hold or be eligible for a Medicare card.
Vaccines recommended during pregnancy can help protect you from serious illness and complications while you’re pregnant. They also provide early protection for your baby.
If you are already vaccinated for COVID-19, you do not need to be vaccinated again during pregnancy. You can still choose to have the COVID-19 vaccine if that is your preference, or if you are in a high risk group.
If you are travelling during pregnancy to certain countries, extra vaccinations might be recommended. If you have questions about vaccination during pregnancy, speak to your doctor or midwife.
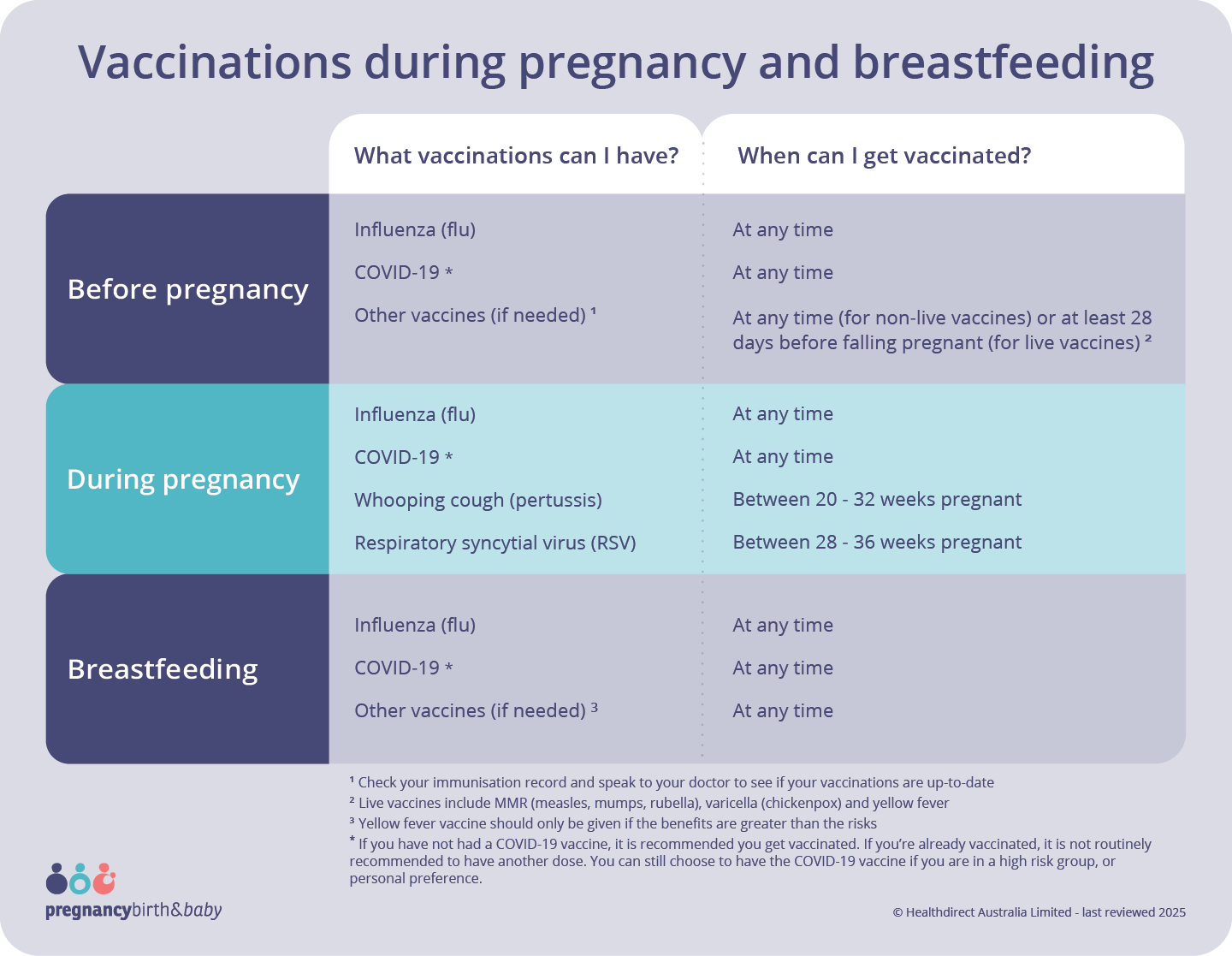
View text version of infographic
Vaccinations during pregnancy and breastfeeding
What vaccinations can I have? And when can I get vaccinated?
Before pregnancy:
- Influenza (flu) - can get at any time
- COVID-19* - can get at any time
- Other vaccines (if needed) 1 - at any time (for non-live vaccines) or at least 28 days before falling pregnant (for live vaccines) 2
During pregnancy:
- Influenza (flu) - can get at any time
- COVID-19* - can get at any time
- Whooping cough (pertussis) - between 20 and 32 weeks pregnant
- Respiratory syncytial virus (RSV) - between 28 and 36 weeks pregnant
Breastfeeding:
- Influenza (flu) - can get at any time
- COVID-19* - can get at any time
- Other vaccines (if needed) 3 - can get at any time
1 Check your immunisation record and speak to your doctor to see if your vaccinations are up-to-date
2 Live vaccines include MMR (measles, mumps, rubella), varicella (chickenpox) and yellow fever
3 Yellow fever vaccine should only be given if the benefits are greater than the risks
* If you have not had a COVID-19 vaccine, it is recommended you get vaccinated. If you’re already vaccinated, it is not routinely recommended to have another dose. You can still choose to have the COVID-19 vaccine if you are in a high risk group, or personal preference.
Which vaccinations are not recommended during pregnancy?
Some vaccines are not recommended during pregnancy because they contain a tiny amount of live (but weakened) virus.
These include vaccinations against:
- MMR (measles, mumps, rubella)
- varicella (chickenpox)
- yellow fever
There is a very small chance that the live virus in the vaccine could pose a risk to your unborn baby. This is why it’s recommended to check that you are up to date with all your vaccinations if you are planning a pregnancy. It’s best to have these vaccinations at least 4 weeks before you become pregnant.
The human papillomavirus (HPV) vaccine is also not recommended during pregnancy. If you have started the course of HPV vaccines and become pregnant, you should continue the course only after your baby is born.
Before getting a vaccination, be sure to let your doctor or health professional know if you may be pregnant.
Are there side effects from vaccinations?
Side effects from vaccines are usually mild and short-lasting. You might have a sore arm or mild swelling where you had the injection. You may also have a mild fever or feel unwell.
Most mild side effects last only for a few days, and are part of the body’s natural response to the vaccine.
Serious or long-lasting side effects are very rare.
Talk to your doctor about the side effects of the vaccine so you know what to expect.
If you have any severe side effects, get medical help straight away by calling triple zero (000) and asking for an ambulance.
How much do vaccinations in Australia cost?
The cost of vaccination in Australia varies.
Many vaccines are free under the National Immunisation Program (NIP). The NIP includes a range of immunisations given throughout your life, from childhood to adulthood. You can access these if you have Medicare.
Your doctor or pharmacist may charge a fee to give the vaccine, even if the vaccine is free. It’s a good idea to check the costs with your health provider when you book your appointment.
What is the Australian Immunisation Register (AIR)?
Australia has a national register for vaccinations. This is called the Australian Immunisation Register (AIR). It helps you keep track of your and your child’s immunisations.
You can get a list of your past vaccines from myGov, or ask your doctor. If you have Medicare, you will automatically be added to the AIR when you have any vaccines.
Resources and support
Vaccination is a personal choice, but an informed choice is always best. If you have questions or need more information about vaccines and pregnancy, you can speak with your doctor directly or call healthdirect on 1800 022 222 (known as NURSE-ON-CALL in Victoria).
Other Australian Government online resources include the following:
To find out what vaccines are recommended for you while you’re pregnant, visit SKAI - Sharing Knowledge About Immunisation.
Languages other than English
The Australian Government has videos and factsheets on vaccinations during pregnancy, available in many community languages.
Health Translations Victoria has brochures on the whooping cough (pertussis) vaccine during pregnancy and on vaccine side effects, both available in many community languages.
Information for Aboriginal and/or Torres Strait Islander peoples
The Australian Government has videos, fact sheets and posters on vaccination during pregnancy for Aboriginal and/or Torres Strait Islander people.
NSW Health has information on which vaccinations are recommended for pregnancy for Aboriginal and/or Torres Strait Islander people.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2025









