Asthma in children under 6
12-minute read
Asthma can be life-threatening — if your child is finding it hard to breathe, take them to the nearest hospital emergency department or call triple zero (000) for an ambulance.
Key facts
- Asthma is a respiratory (lung) condition that can make your child’s airways become narrow at times.
- The symptoms of asthma include wheezing, difficulty breathing and coughing.
- In children, the most common trigger for asthma is a viral infection, such as a cold.
- Your doctor can usually diagnose asthma, and may recommend your child starts a treatment to help with their symptoms.
- It’s important that your child has a written asthma action plan — this will help you manage their asthma and know what to do if they have an asthma attack.
What is asthma?
Asthma is a respiratory condition that causes your child’s airways to become narrow. This is due to:
- the lining of their airways becoming swollen and inflamed
- the layer of muscle inside their airways becoming tight
- their airways being blocked by mucus
Asthma affects 1 in 5 children.
Wheezing is the most common symptom of asthma in children under 5 years of age. Wheezing is a high-pitched sound coming from your child’s chest when they breathe in and out.
Not all children with wheezing have asthma. In children younger than 12 months of age, wheezing is usually caused by bronchiolitis (lung infection).
What are the symptoms of asthma in children?
Symptoms of asthma in children can include:
- wheezing — this is most noticeable when your child breathes out
- coughing — this often occurs at night or when waking up in the morning
- difficulty breathing — you may notice the skin above your child’s collarbone being sucked in as they breathe
- breathing faster than normal
- chest tightness — this is when your child's breathing seems 'tight' or they are short of breath
Your child doesn’t have to have all these symptoms to have asthma.
The symptoms of asthma can range from mild to severe.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes asthma?
The exact cause of asthma is not known.
Asthma can be genetic, which means many children with asthma have a family history of asthma.
Asthma symptoms can be triggered by many things. The most common trigger is an infection, such as a cold or the flu.
Your child’s symptoms may be triggered by an allergy to:
- pollen
- animal dander (dead skin and fur), usually from pets
- mould
Other triggers for asthma include:
- exercise
- cold, dry air
- changes in the air environment (such as thunderstorms and bushfire smoke)
- cigarette smoke
- air pollution
You can prevent asthma symptoms by helping your child avoid triggers.
When should I see my doctor?
You should see your doctor if your child has wheezing, or other symptoms of asthma.
When to seek urgent care
If your child is finding it hard to breathe, take them to the nearest hospital emergency department or call triple zero (000) for an ambulance.
Get urgent medical attention if your child:
- is not breathing
- is having difficulty breathing — you may notice your child breathing rapidly or moving their chest a lot
- is unable to speak normally
- has slightly blue lips — this is a sign that not enough oxygen is reaching their body
- is having an asthma attack and a reliever is not available
- has asthma symptoms that do not get better with asthma medicines
- is distressed or confused
A severe asthma attack can be very upsetting because your child will feel like they can’t get enough air.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is asthma diagnosed?
Your doctor can usually diagnose asthma.
Your doctor will ask about your child’s symptoms. Your doctor will also want to know:
- what brings on your child’s symptoms
- what time of day your child has symptoms
- how often your child has symptoms
- about your child’s general health, including any allergies
- whether your child is exposed to smoke in your home
- whether anyone in your family has asthma or allergies
- what helps with your child’s symptoms
Your doctor will examine your child and listen to their breathing with a stethoscope. They may also check your child’s heart rate and blood pressure.
If your doctor is unsure what is causing your child’s symptoms, they may suggest getting a chest x-ray. They may also refer your child to a paediatrician (children’s doctor).
If your doctor thinks that your child has asthma, they may recommend a treatment trial. This means they will give your child asthma medicines, to see if this helps with your child’s symptoms.
How is asthma treated?
There are 2 main types of asthma medicines, known as 'relievers' and 'preventers'.
Relievers
These can help reduce your child’s asthma symptoms when they happen. The most common reliever medicine is salbutamol (a well-known brand is Ventolin).
All children should use reliever medicine to help with severe asthma symptoms or an asthma attack, even if they also take preventer medicine.
Preventers
These help reduce how often your child has asthma symptoms. Preventers can be used in children with asthma who have:
- symptoms that happen regularly (like having daytime symptoms twice a week or more)
- symptoms that make it hard for them to play or sleep
- 2 or more flare-ups while taking other oral asthma medicines
Preventer medicines need to be taken every day, even when your child is feeling well. Some preventer medicines are taken as inhalers (breathed in through the lungs), while others are taken as a tablet.
Asthma medicines are often taken using an inhaler and a device called a spacer. It’s important to learn how to use an inhaler and spacer properly.
Your child will need regular follow-up visits with your doctor. This is to check on their symptoms and decide if they still need treatment. It can be helpful to write down what caused your child’s symptoms and when they took their asthma medicine. This can help your doctor work out if changes to medicines are needed.
Asthma action plan
Ask your doctor to create a written asthma action plan for your child. An asthma action plan helps you manage your child’s asthma. It lists:
- your child’s usual medicines
- when and how your child should take their medicine
- what to do if your child’s symptoms get worse
- what to do in the case of an asthma emergency
Share your child’s asthma action plan with everyone who cares for your child, including:
- childcare workers
- friends
- family members
LOOKING FOR A MEDICINE? — To search by brand name or active ingredient, use the Medicines information search feature.
Managing an acute asthma attack
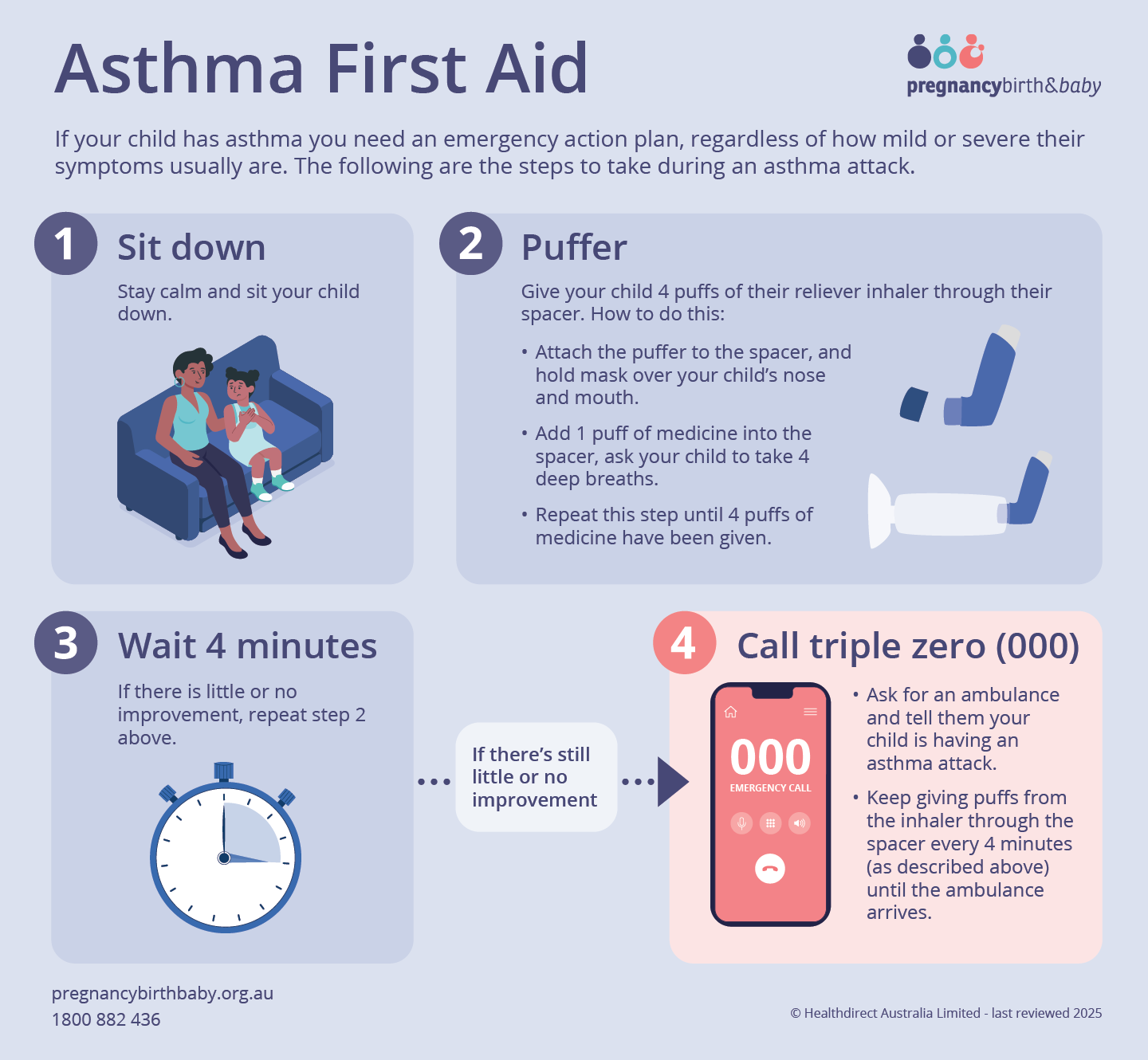
If your child has asthma, you need an emergency action plan, even if their symptoms are usually mild.
If your child has a severe asthma attack:
- Stay calm and sit your child down.
- Put 1 puff into their spacer. Give your child 4 breaths of their reliever inhaler through their spacer.
- Repeat this process until 4 separate puffs have been taken.
- Wait 4 minutes. If there is little or no improvement, repeat step 2.
- If there is still little or no improvement after 4 minutes, call triple zero (000) and ask for an ambulance. State that your child is having an asthma attack.
While waiting for the ambulance to arrive, give your child puffs from the inhaler through the spacer as instructed above. Wait 4 minutes and do it again. Repeat this until the ambulance arrives.
Can asthma be prevented?
Asthma can’t be prevented entirely, but there are ways to lower your child’s chance of having asthma symptoms.
You should avoid smoking and exposure to cigarette smoke while pregnant. Smoking and breathing in second hand smoke during pregnancy can affect your baby’s lungs. This can increase your child’s chance of having asthma.
Asthma symptoms can sometimes be prevented by avoiding triggers. For example, if you know that animal dander (dead skin and fur) triggers your child's asthma, reducing animal hair in your home can help.
It’s recommended that your child is up to date with their vaccinations. This can help protect them from respiratory infections, which can cause asthma symptoms. Talk to your doctor or child health nurse about which vaccinations your child may need.
What are the complications of asthma?
Children with asthma can have severe symptoms or asthma attacks.
Children with severe asthma symptoms may need to go to hospital for treatment. In some cases, severe asthma symptoms can cause respiratory failure (lung failure).
It’s important to manage your child’s asthma well to help prevent severe asthma symptoms and asthma attacks.
Should my child with asthma be active?
It’s important for children with asthma to be active. This will help them stay fit and healthy.
Talk with your doctor about how to prevent and manage asthma symptoms when your child is active. Your child's asthma action plan will help with this.
Resources and support
The National Asthma Council's Australian Asthma Handbook has:
- information on diagnosing asthma in children 1 to 5 years of age
- a summary of asthma management in children 1 to 5 years of age
Asthma Australia has:
- a first aid fact sheet on what to do if your child has an asthma attack
- information on what is included in an asthma action plan
- resources in languages other than English
- videos on how to use your medicines
Call the Asthma Australia Information Line on 1800 278 462 to talk to an Asthma Educator.
Log on to the Asthma Buddy app to help keep track of your child's symptoms.
You can call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with you 24 hours a day, 7 days a week.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2025






-537d5d.png)
